
Myopathic MUAPs‡ with fibrillation potentials∥ Gottron papules heliotrope rash calcinosis interstitial lung disease disordered GI motilityĮlevated myoglobin ANA positive myositis autoantibodies may be present With or without myopathic MUAPs‡ and fibrillation potentials∥ Menorrhagia bradycardia goiter delayed relaxation of deep tendon reflexes
Myopathic MUAPs‡ with or without fibrillation potentials∥ Weight loss tachycardia increased perspiration tremorĮlevated T 4 and T 3 TSH variable, depending on cause Usually has associated comorbidities (cardiovascular disease, diabetes)Ītrophy of type II muscle fibers increased lipofuscin beneath cell membrane calcium deposits in muscle Proximal, lower extremity more than upper extremity Parathyroid hormone (secondary hyperparathyroidism§) Selective atrophy of type II muscle fibers Hyponatremia hyperkalemia ACTH assay ACTH stimulation testĮlevated urine-free cortisol, dexamethasone suppression, or corticotropin-releasing hormone stimulation tests
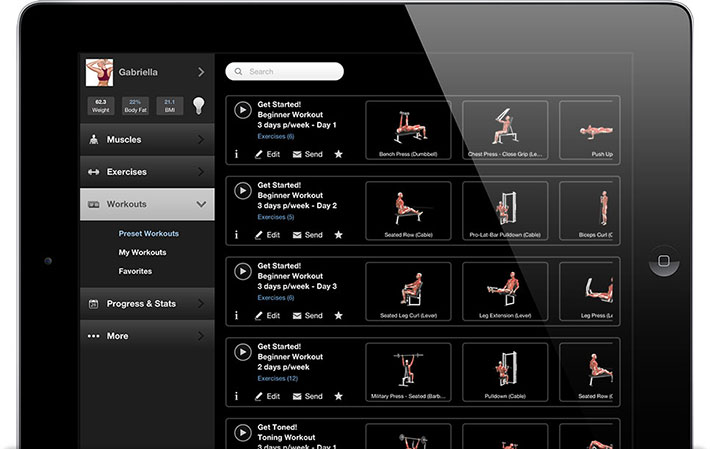
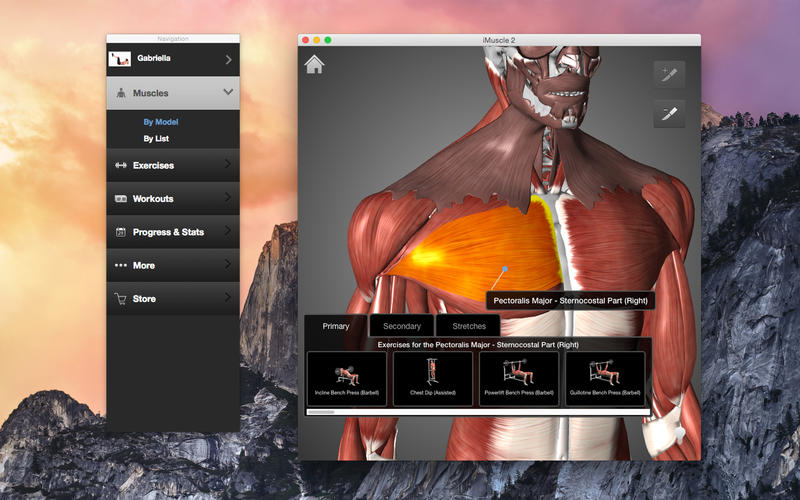
#Imuscle 2 review skin
Hypotension hypoglycemia bronzing of the skin Myopathic changes* selected atrophy of type II muscle fibers 13, 27 – 30Ĭhange in mental status telangiectasia peripheral neuropathyĮlevated transaminase and GGT levels anemia decreased vitamin B 12 Patients in whom these disturbances are suspected should have electrocardiography to screen for cardiac sequelae. 17, 18 Disorders of potassium balance are among the more common electrolyte myopathies and may be primary (such as in hypokalemic or hyperkalemic periodic paralysis) or secondary (such as in renal disease or angiotensin-converting enzyme inhibitor toxicity). 21 – 23 Rheumatologic disorders causing weakness, such as systemic lupus and rheumatoid arthritis, can occur in young and elderly persons. 14, 15, 32 Inflammatory diseases typically affect older adults and include both proximal (polymyositis and dermatomyositis) and distal myopathies (inclusion body myositis) the proximal inflammatory myopathies respond to steroids. Of the endocrine diseases, thyroid disease is common, but thyroid-related myopathy is uncommon parathyroid-related myopathy should be suspected in a patient with muscle weakness and chronic renal failure. Less common myopathies include those caused by endocrine, inflammatory, rheumatologic, and electrolyte syndromes ( Tables 4 5 – 8, 13 – 26 and 5 6, 8, 15, 16, 18, 20, 24 – 38). Pathologic evaluation of the muscle tissue specimen focuses on histologic, histochemical, electron microscopic, biochemical, and genetic analyses advances in technique have made a definitive diagnosis possible for many myopathies. Finally, many myopathies require a biopsy for diagnosis. Physicians should begin with blood chemistries and a thyroid-stimulating hormone assay to evaluate for electrolyte and endocrine causes, then progress to creatine kinase level, erythrocyte sedimentation rate, and antinuclear antibody assays to evaluate for rheumatologic, inflammatory, genetic, and metabolic causes.
If the diagnosis remains unclear, the examiner should pursue a tiered progression of laboratory studies. Otherwise, electromyography is indicated to confirm the presence of a myopathy or to evaluate for a neuropathy or a disease of the neuromuscular junction. If a specific cause of weakness is suspected, the appropriate laboratory or radiologic studies should be performed. In the physical examination, the physician should objectively document the patient’s loss of strength, conduct a neurologic survey, and search for patterns of weakness and extramuscular involvement.

The pattern and severity of weakness, associated symptoms, medication use, and family history help the physician determine whether the cause of a patient’s weakness is infectious, neurologic, endocrine, inflammatory, rheumatologic, genetic, metabolic, electrolyte-induced, or drug-induced. Diagnosis begins with a patient history distinguishing weakness from fatigue or asthenia, separate conditions with different etiologies that can coexist with, or be confused for, weakness. Muscle weakness is a common complaint among patients presenting to family physicians.


 0 kommentar(er)
0 kommentar(er)
